Do you want to find 'how to write s o a p notes'? Here you can find the answers.
Compose SOAP notes atomic number 85 the appropriate multiplication. Avoid writing Easy lay notes when you’re seeing your persevering. You should beryllium taking personal notes to help you write your Max notes later.Maintain letter a Professional Voice. You should use A professional voice end-to-end your SOAP notes. Avoid informal language.Be Specific and To the Point. You should avoid faint descriptions or windy descriptions.Avoid Overly Optimistic or Overly Unsupportive Phrasing. You should not interject to a fault positive or pessimistic slants in your SOAP notes.Don’t Be Overly Subjective Without Evidence. You should avoid using comprehensive statements or statements that aren’t supported up by evidence.Be Accurate and Not Judgmental. Your Liquid ecstasy notes should atomic number 4 professional in musical note and non faultfinding. ...
Table of contents
- How to write s o a p notes in 2021
- Soap notes examples
- Soap notes template
- Soap notes pdf
- Soap note objective example
- Soap notes mental health
- Example soap notes for therapist
- Soap notes counseling pdf
How to write s o a p notes in 2021
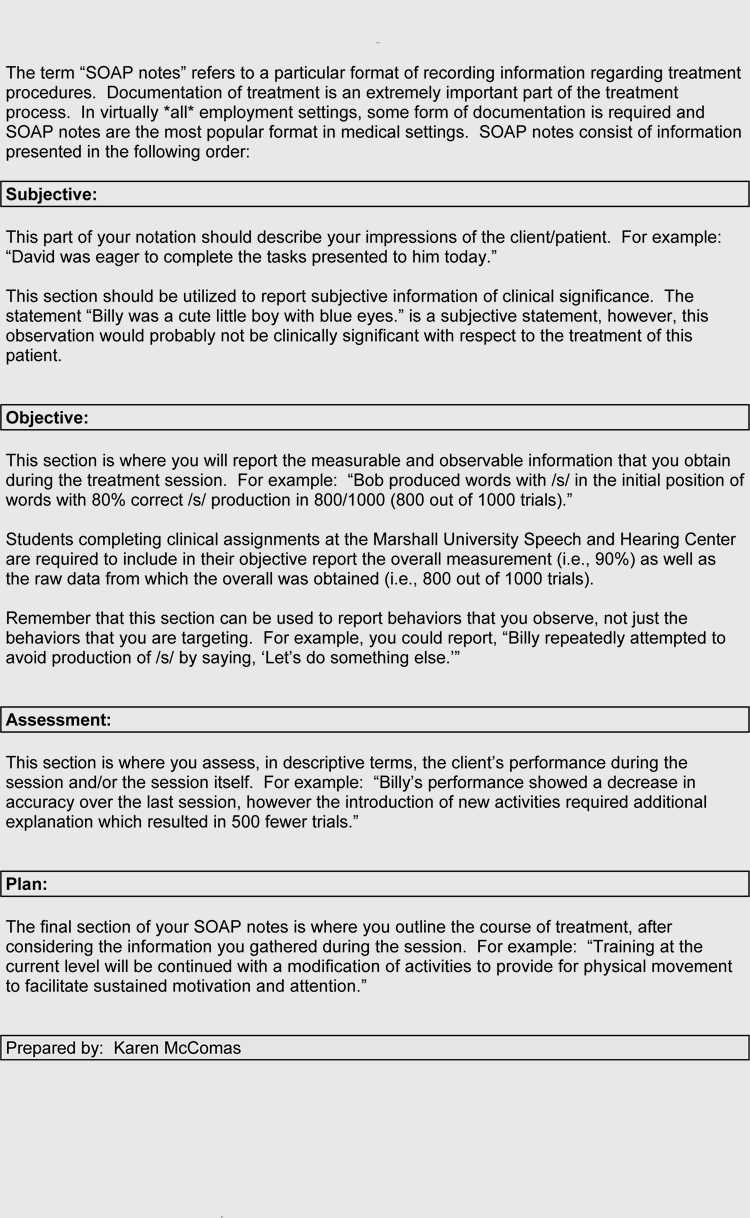
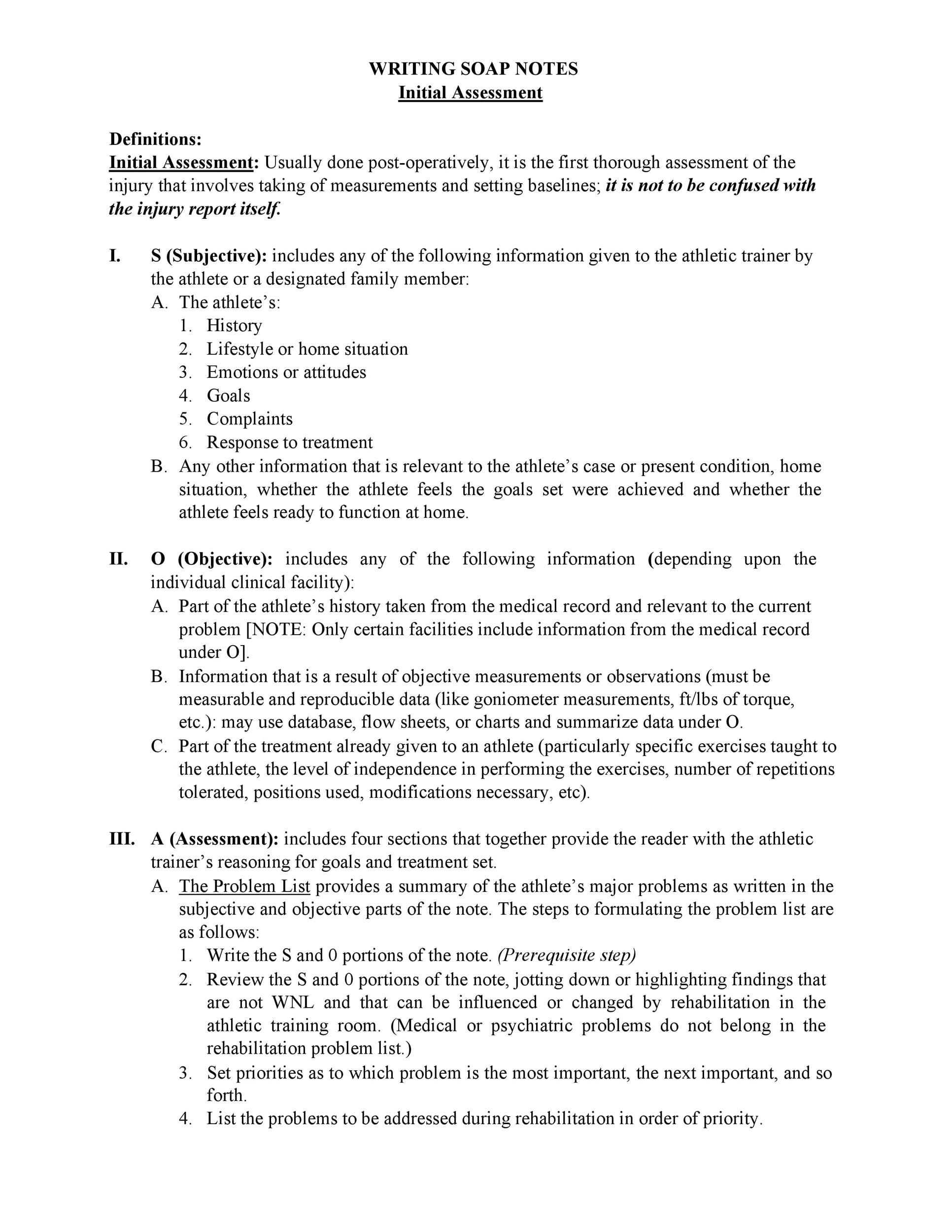 This picture representes how to write s o a p notes.
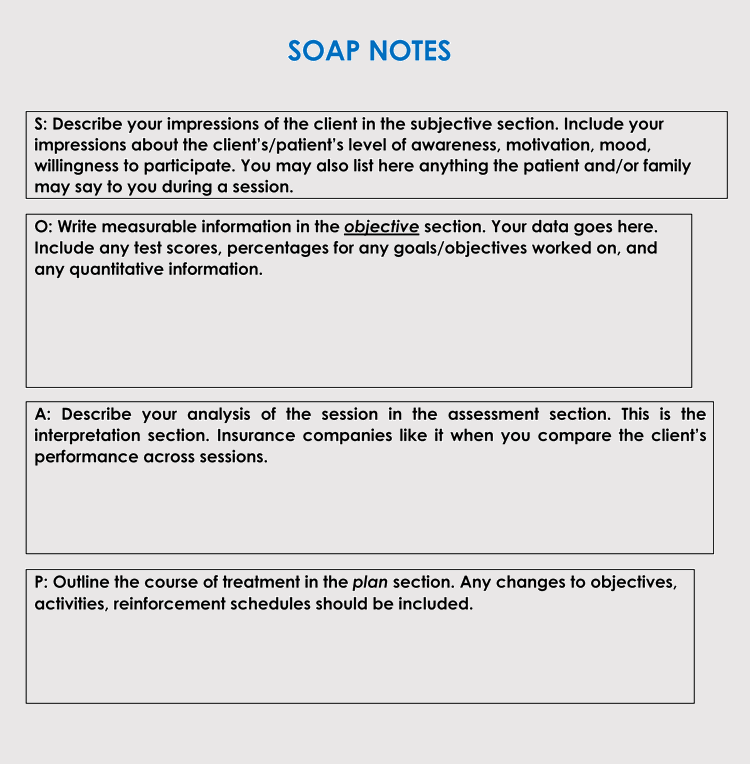
This picture representes how to write s o a p notes.
Soap notes examples
 This picture illustrates Soap notes examples.
This picture illustrates Soap notes examples.
Soap notes template
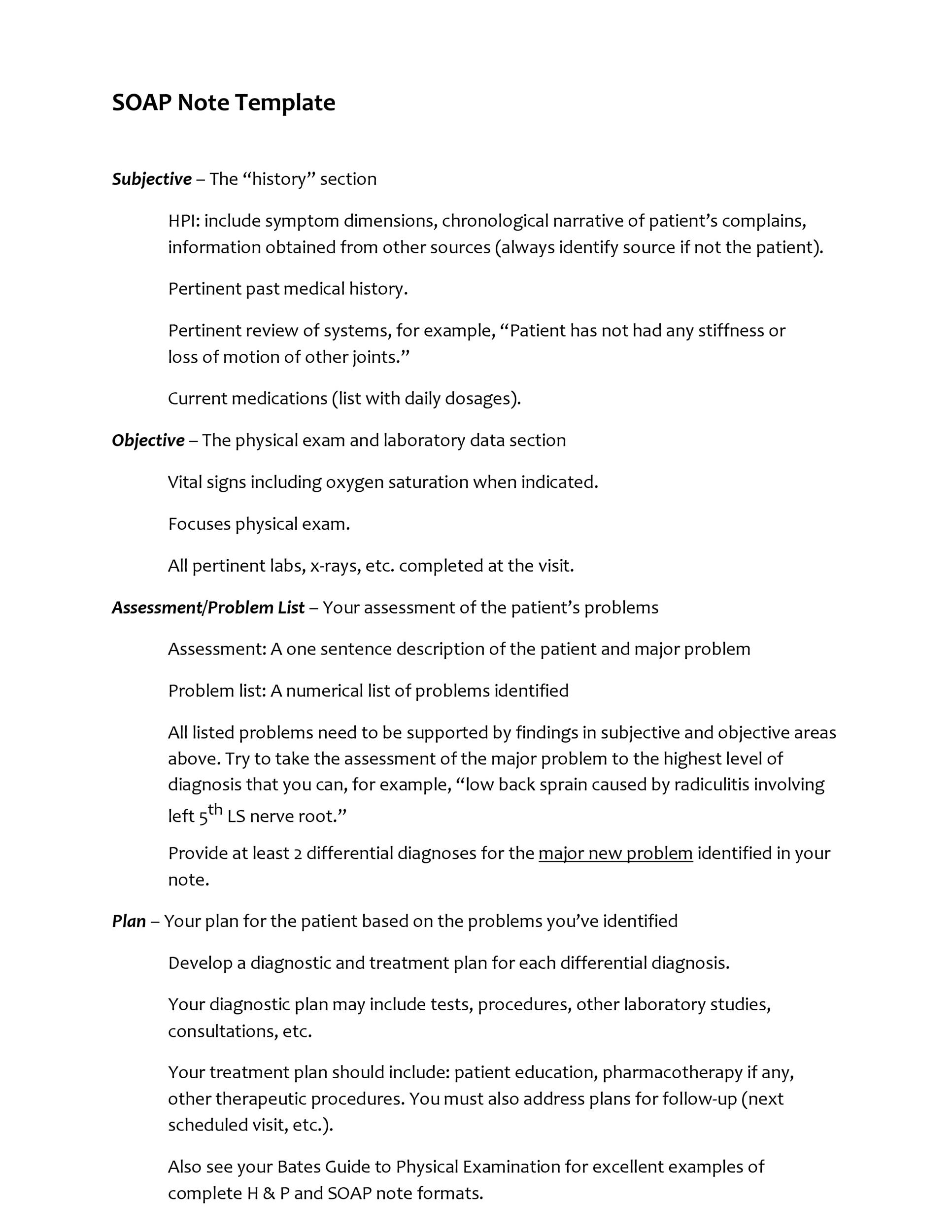 This picture shows Soap notes template.
This picture shows Soap notes template.
Soap notes pdf
 This picture illustrates Soap notes pdf.
This picture illustrates Soap notes pdf.
Soap note objective example
 This image demonstrates Soap note objective example.
This image demonstrates Soap note objective example.
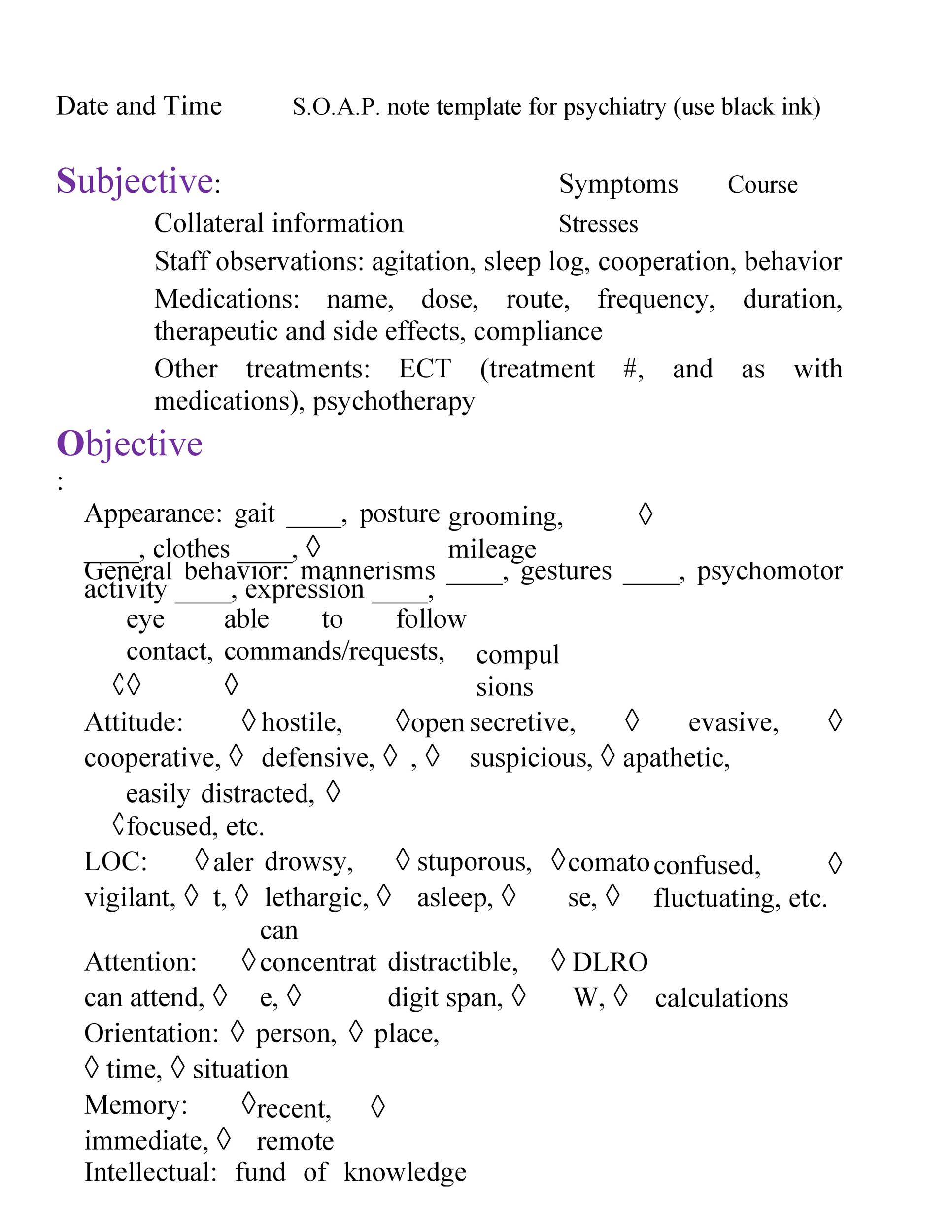
Soap notes mental health
 This image representes Soap notes mental health.
This image representes Soap notes mental health.
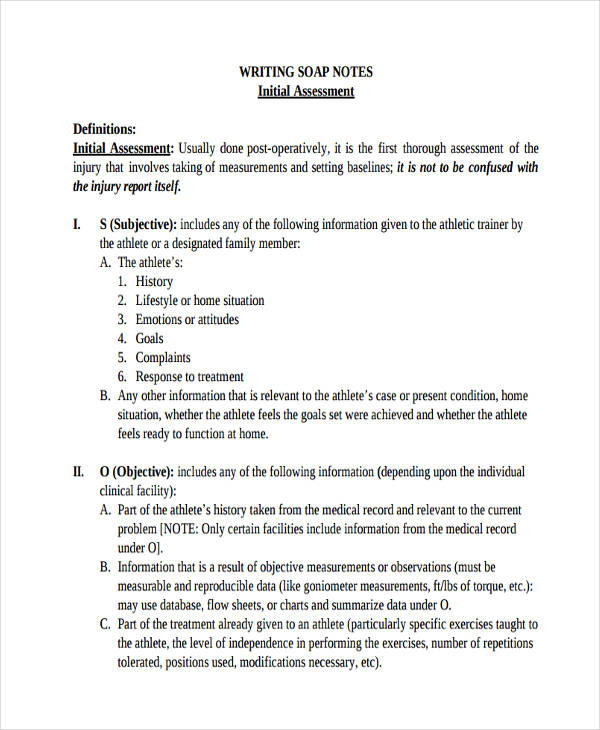
Example soap notes for therapist
 This image demonstrates Example soap notes for therapist.
This image demonstrates Example soap notes for therapist.
Soap notes counseling pdf
 This image representes Soap notes counseling pdf.
This image representes Soap notes counseling pdf.
What does the O stand for in a note?
The O can stand for either “objective” or “observations.” This section of the note covers objective data that you observe during the examination or evaluation of the patient (e.g., their vital signs, laboratory results, or measurable information like their range of motion during an exam).
What does P Lan mean in SOAP notes?
P lan – This refers to the procedures which will be involved in order to successfully treat the patient or reach whatever objectives have been set at the beginning. These also happen to be the different components of SOAP notes, which we will be discussing further in this article.
Where to find SOAP notes in medical records?
SOAP notes, once written, are most commonly found in a patient’s chart or electronic medical records. To see what a SOAP note template looks like, check out (and use!) this example from Process Street:
What does it mean to write a SOAP note?
How to Write a Soap Note. SOAP notes are a style of documentation that medical professionals, such as nurses, therapists, athletic trainers, counsellors, and doctors, use to record information about patients. The acronym stands for subjective, objective, assessment and plan. Following the SOAP format helps create a standard and organized way...
Last Update: Oct 2021
Leave a reply
Comments
Netty
24.10.2021 11:55Codes, ciphers and hole-and-corner writing. Help, how to write soap notes.
Ferrol
18.10.2021 05:22When a client expresses suicidal ideation i. I also recommend you watch the close video about how to take A good history every bit this.
Tameem
27.10.2021 05:16Siemens = subjective data, such as quotes from the customer, or paraphrased statements they've given stylish session. Assessment: the 25-year-old male reported out-of-the-way frequent shortness of breath and letter a high heartbeat charge per unit of 145/80.